Healthcare
Patient tracker and composite healthcare for NHS using hl7 data integration
Introduction
Various hospitals and government health care entities capture their patient’s health records and logs. The data traditionally sits in different systems and in different formats. There has been a need for sharing the records or interoperate with different systems, hospitals, clinics, doctors or event government organizations. Hl7 standard has been there for some time which opens a door for such possibilities through a software system and set of APIs. However, this is quite a challenging piece of work and there are complexities involved which need to be solved thoroughly before such a system can be designed.
- Health care data follows hl7 standard and it is extremely complex in nature. Most of the existing systems find it very hard to process the data. Look at an example of hl7 data
- The data is nested, there are whole set of structuring and constraints that need to be followed as per hl7 guidelines. It is very hard to process such data.
- Following is the high-level requirement for such system
- The data is connected and potential of improving the intelligence is huge - therefore Graph structuring is required for most of the data apart from document, and text data processing
- Data moves in real-time, therefore, we need to capture, process, act and store in real-time in continuous manner. Need for real-time stream/timeseries processing is needed
- Large data or binary data should also be stored and indexed. Secondary and Reverse indexing is required for high-speed retrieval or query
- Vector indexing is needed for similarity (semantic) use cases – which is extremely important for various reasons in the system
- High performance, huge scale, privacy, security, encryption, disaster recovery, replication etc. are first set of requirements for such system
- User interfaces with charts, dashboards and interactive UI workflows for performance several actions
- REST API for integration with other systems. Cloud or om-prem or hybrid deployments
What is hl7 standard?
HL7 stands for Health Level Seven International. It's a set of international standards for the exchange, integration, sharing, and retrieval of electronic health information. These standards define a framework for the exchange, management, and integration of electronic health information between various healthcare systems. HL7 standards are widely used in healthcare IT systems to ensure interoperability and facilitate the exchange of clinical and administrative data between different healthcare organizations and systems.
Why hl7 standard?
- Interoperability: HL7 standards provide a common framework for structuring and exchanging healthcare information, regardless of the systems or applications used by different healthcare organizations. This interoperability is essential for improving care coordination, enhancing patient safety, and supporting clinical decision-making
- Data Exchange: HL7 enables the exchange of a wide range of healthcare data, including patient demographics, clinical observations, laboratory results, medications, and administrative information. This data exchange is vital for facilitating communication between different healthcare providers, such as hospitals, clinics, laboratories, pharmacies, and public health agencies.
- Standardization: HL7 promotes standardized formats and protocols for representing and transmitting healthcare information. By adhering to these standards, healthcare organizations can ensure consistency in data exchange, reduce errors, and improve the efficiency of healthcare processes
- Integration: HL7 standards support the integration of disparate healthcare systems and applications, allowing them to work together seamlessly. This integration enables healthcare providers to access and share patient information across different systems, improving workflow efficiency and continuity of care.
- Regulatory Compliance: HL7 standards are often required or recommended by regulatory bodies and healthcare organizations to ensure compliance with healthcare IT regulations and standards. Adhering to HL7 standards can help healthcare organizations meet regulatory requirements related to data exchange, interoperability, and patient privacy and security.
- Facilitating Innovation: By providing a standardized framework for exchanging healthcare information, HL7 encourages innovation in healthcare IT solutions and interoperable healthcare systems. Developers can build applications and solutions that leverage HL7 standards, enabling new capabilities and functionalities to improve patient care and healthcare delivery.
The problem
Data exchange between different systems in healthcare is a complex subject. The widespread adoption of EHR systems and the digitalization of administrative processes within many healthcare organizations has resulted in large amounts of data.
Managing such a vast and intricate volume of data posed a significant challenge for existing systems. Moreover, retrieving the necessary information became an even more daunting task atop this complexity.
Challenges
- Complexity: HL7 data is inherently complex, with numerous interdependencies between data elements. We must contend with parsing and interpreting this intricate data structure accurately.
- Scalability: As the volume of HL7 data continues to grow, we must ensure that its systems can scale effectively to handle the increasing data load without sacrificing performance or reliability.
- Interoperability: HL7 data often needs to be integrated with various other systems and formats within healthcare environments. we must ensure seamless interoperability between HL7 data and other data formats or standards to facilitate smooth data exchange and workflows.
- Security and Privacy: Healthcare data, including HL7 messages, is subject to stringent security and privacy regulations. We must implement robust security measures to safeguard HL7 data from unauthorized access, breaches, or data leaks.
- Data Quality: Maintaining the quality and integrity of HL7 data is crucial for accurate clinical decisionmaking and patient care. We must implement data validation and cleansing processes to ensure that HL7 data is accurate, complete, and consistent.
- Performance: Processing HL7 data in real-time or near real-time to support critical healthcare workflows requires high-performance computing infrastructure and optimized algorithms. we must continually optimize its systems and algorithms to deliver timely and responsive HL7 data processing capabilities.
Why are existing systems not enough?
With the inherent complexity of HL7 data, existing systems face challenges in storage and processing. The sheer volume and intricate interconnections within this data pose significant hurdles. Executing data operations or running complex queries demands substantial time and resources.
Consequently, developing a user interface atop such a system becomes time-consuming, and crafting queries to extract necessary data adds further complexity.
Solution
Hl7 data demonstrates a high degree of interconnectedness and complexity, adopting a graph-based storage model, composed of nodes and relationships, offers a superior representation of the data. This approach enhances both the storage efficiency and the comprehension of the dataset's structure and interrelations.
Benefits
- Interconnectedness and Complexity: HL7 data, are characterized by intricate relationships and dependencies among various data elements. Storing such data in traditional formats may lead to inefficiencies and difficulties in understanding the underlying connections.
- Graph-based Storage: By organizing the data as a graph, where nodes represent individual data points and relationships denote the connections between them, the inherent complexity of the dataset can be captured more accurately. This model provides a visual and intuitive representation of the data's interconnections.
- Storage and Understanding: Storing the data as nodes and relations within a graph not only optimizes storage space but also enhances data comprehension. The graphical representation allows analysts and stakeholders to visualize the relationships between different data points, facilitating a deeper understanding of the dataset's structure and dynamics.
- Query Complexity: By organizing data in this graph format, querying becomes more straightforward as it aligns with the inherent structure of the information, making it easier to traverse and extract relevant data points.
- Retrieval time: Retrieval time for data is notably reduced compared to traditional storage methods, as the graph structure enables more efficient navigation through interconnected data elements
- Data Accuracy: The adoption of this storage approach not only improves operational efficiency but also enhances the accuracy of the data by preserving its inherent relationships and dependencies.
- Flexibility: Graph databases are schema-less or have flexible schemas, allowing for dynamic changes in data structure without requiring a predefined schema. This flexibility is advantageous for accommodating the evolving nature of HL7 standards and healthcare data.
- Efficient Querying: Graph databases excel at traversing relationships between data entities, making complex queries more efficient and performant. This capability is particularly valuable for healthcare applications where queries often involve navigating through interconnected data elements.
- Real-Time Insights: Graph databases enable real-time analysis and insights by providing fast query response times, even with large and interconnected datasets. This rapid querying capability is crucial for supporting decision-making processes in healthcare environments where timely information is critical.
- Interoperability: HL7 data often needs to be integrated with data from other sources, such as electronic health records (EHRs) or medical imaging systems. Graph databases facilitate seamless integration by providing a unified platform for storing and querying heterogeneous healthcare data.
- Scalability: Graph databases are inherently scalable, capable of handling growing volumes of HL7 data with ease. As healthcare data continues to proliferate, the scalability of graph databases ensures that performance remains consistent even as the dataset size increases.
Solution Details
Entities
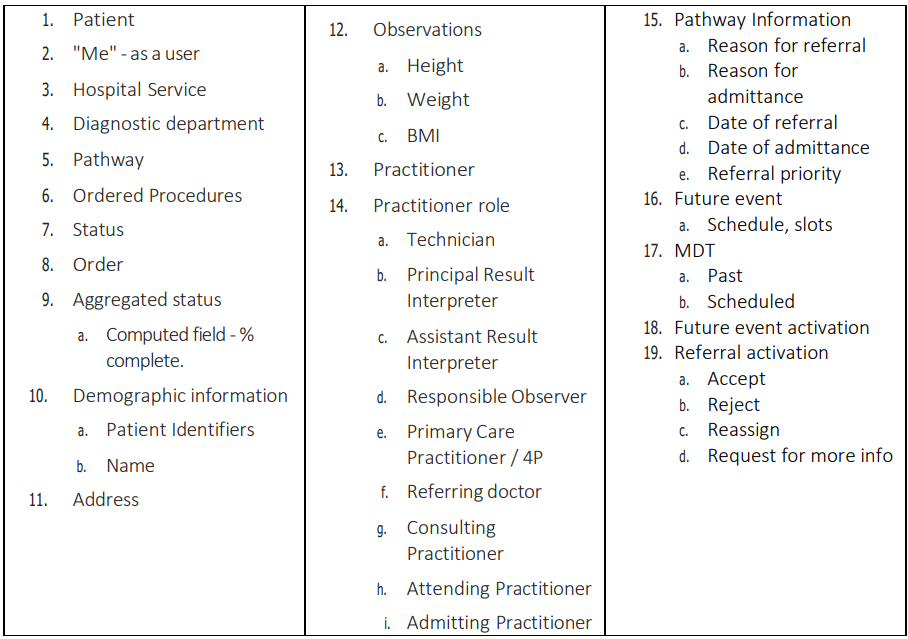
Patient Tracker
As a user, we should be able to view list of patients that are related to
- Me
- My hospital service
- A schedule MDT
- That is related to me (my MDT’s) or my hospital service
- For each of the patients, we should be able to see the status of their ordered procedures, grouped by hospital service
A computed field is needed that determines the % of the ordered procedures that related to the specific order and diagnostic department/hospital service that have the status F or COMPLETE
For each of the patient also we need to be able to view following
- Full name
- Patient id
- Birth date
- Address
- Primary care practitioner (GP)
For each Patient,we also need to have Pathway information asitrelatesto the User’srelationship with patient
- Date of Admittance or Referral
- Reason for Admittance or Referral ,
- PreviousMDT"date"
- Scheduled for MDT "date"
- Key Practitionersthat are involved (by Role).
For each patient, we also need to have key observations
- Height
- Weight
- BMI
Patient Tracker - Orders and Results - Line Item modal
1. When I click on the individualstatuses ofthe ”aggregated status", I need to see/accessthe line item (can these line items be expandable assome ofthisis only needed ifthere is an exception)
- Ordered Procedures,
- Their Status,
- The ordered date
- Last updated
- Practitioners by Role (Technician, Principal Result Interpreter. Assistant Result Interpreter, Responsible Observer)
2. Create schedule and slots future event
- As a user, I need to be able to create future eventslike clinic's, MDT's etc and to be able to add dates, start and finish times, as well asthe number of available slots.
- I also need to be able to add detailslike the location and URL forthe online meeting.
- I also need to be to add Practitioners and attendeesfroma list ofsystem users/ user groups.
3. Patient Tracker Add to future event
- As auser,” whenI click theAddto future event, open amodaltoallowme toadd the patient to a scheduled (future) event via a Calendar view or a filterable drop down"
4. Patient Tracker - Future event Dashboard
- For example, in MDT'sitsthe % of completed tests/results/appointments
- For othersituations, it could be the number of patientswho have responded to an invitation to book an appointment
As a user, I need to be able toviewupcoming MDT's(that are related tome/my hospital service) and the aggregated value of howmany patients are ”ready for event"
5. Patient Tracker - Referral Management
- me
- my hospital service,
- Full Name
- Patient Id
- Date of birth
- Address-unlessthe patient hasthe Consent Type "LocationHiding"> =1. Ifthe patient has this consent type then address/phone/email etc fields should not be returned.
- PhoneNumber - unlessthe patient hastheConsent Type "LocationHiding" >=1. Ifthe patient hasthis consent type then address/phone/email etc fieldsshould not be return
- Their Primary Care Practitioner (GP) - Consent Type "Location Hiding" >=1. If the patient has this consent type then GP should not be returned.
As auserIneedtobe able toviewa list ofreferralsthat are related to
For eachPatient alsoneedto be able toviewtheir properties
For each Patient,we also need to have Pathway information asitrelatesto the user’s relationship with patient
- Date of referral
- Reason for referral
- Referral priority
- Key Practitionersthat are involved (by Role)
As a user I need to be able accept, reject or reassign the referral or request additional information from the referring doctor.
Composite care record
All information related to the patient and their history